Peptone Basic Information
Peptone Structure
Peptone Water,Peptone Composition,Peptone Water Composition,Peptone Meaning,Peptone Water Preparation ShanDong YingLang Chemical Co.,LTD , https://www.sdylhgtrade.com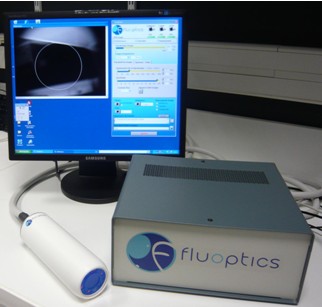


CAS: 73049-73-7
MF: C13H24O4
MW: 244.32726
EINECS: 615-895-9
Mol File: 73049-73-7.mol
solubility H2O: 50 mg/mL
form powder
color Dark cream powder
Odor Odorless
PH 6.5-7.5 (2% in H2O)
Water Solubility Soluble in water. Insoluble in alcohol.
Sensitive Moisture Sensitive & Hygroscopic
EPA Substance Registry System Peptones (73049-73-7)
Primary breast cancer resection in rats guided by near-infrared fluorescence surgery navigation system
Primary breast cancer resection in rats guided by near-infrared fluorescence surgery navigation system
Incomplete resection of the tumor has been a clinical problem that has plagued breast cancer surgery. In the patients who underwent breast preservation surgery, 5%-40% of patients with resected margins can still detect residual tumors, and have to carry out additional Surgery and radiation therapy. And 10% of patients who have no biopsy confirmed by biopsy continue to be affected by neoplastic disease. Therefore, significantly increasing the rate of surgical resection will increase the success rate of surgery, and real-time monitoring of the surgery removes the obstacles for this vision.
Near-infrared imaging technology is a commonly used imaging technique in laboratories, but it can also be applied to surgery to make tumor cells visible. This provides an excellent tool for surgeons who rely solely on palpation and eye exams to diagnose the condition, and this technique is also used in cases of malignant gliomas and liver cancer. The advantage of near-infrared fluorescence is that it has good tissue penetration, very low autofluorescence, and a good signal-to-noise ratio. Moreover, since the human eye is not sensitive to near-infrared light, the use of near-infrared real-time monitoring surgery does not cause visual interference to the doctor.
The near-infrared real-time monitoring system used in this paper is the near-infrared imaging system fluobeam from Fluoptics, France. It is flexible, portable, real-time monitoring, open imaging, etc., which facilitates our surgery.
To test the performance of this system in breast cancer tumor resection, we used a protease-activated tumor-targeted near-infrared fluorescent probe ProSense 680 and ProSense 750, which are mainly used for observational experiments in surgery and fluorescence microscopy because of its spectrum. It has a good fit to the spectrum of a fluorescent microscope laser; the ProSense 750 is used in non-invasive animal experiments due to its large deviation from the autofluorescence spectrum. Since there are no homologous tumor cells, we planted the tumor mass directly into the rat mammary fat pad and observed the growth state of the tumor after four weeks. Fig1 is the tumor mass under the rat's breast four weeks after tumor implantation.
Fig1
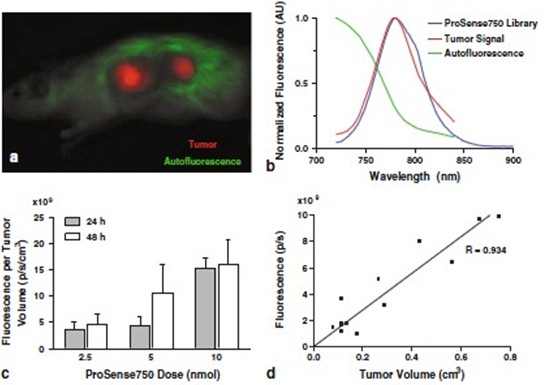
Tumor-specific rats were injected intravenously with the tumor-specific near-infrared probe ProSense750 at a dose of 10 nmol. The distribution of fluorescence in the rats was observed after 24 hours and 48 hours. The tumor fluorescence was observed in the fig2a after 24 hours of probe injection (red). And the distribution of autofluorescence (green), it can also be seen from the spectral analysis that the tumor signal and the spectral signal of ProSense750 have a good fit, and far away from the spectral range of autofluorescence (fig2b). In dose- and time-dependent experiments, we injected 2.5, 5, 10 nmol of fluorescent probes, respectively, and detected them at 24 and 48 hours. The result (fig2c) is a statistical analysis of the fluorescence signals of 35 tumors. Statistically significant, a small 10 nmol measurement of the difference in fluorescence signals between 24 and 48 hours was chosen as the surgical measure. Similarly, the intensity of the fluorescent signal and the actual size of the tumor are also well correlated (fig2d).
Fig2
Under the guidance of the Fluobeam real-time imaging system, we successfully isolated 26 tumors from 7 rats, ProSense 680 was administered at a dose of 10 nmol, and surgery was performed 24 hours after intravenous injection (fig3a). The signal-to-noise ratio of the fluorescence signal and the background averaged 2.35 ± 0.37 (fig3b); during the tumor resection, we reduced the resection of the surrounding tissue as much as possible and tested the accuracy of the fluobeam. In the pathological examination of 17 tumor masses of 5 rats, we found that all of the tumors examined (17) had an average of 1.3 ± 0.6 mm of tumor-free margin and a minimum margin of 0.2 ± 0.2 mm.
Fig3
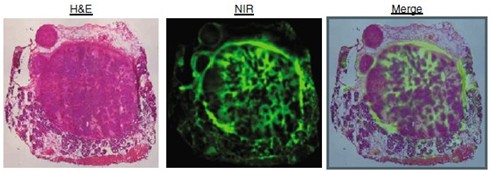
In vitro fluorescence imaging of tumor sections also showed that the signal of the tumor boundary displayed by fluorescence imaging was 1.6 ± 0.3 times stronger than the central signal, which is more conducive to the doctor's determination of tumor boundaries in tumor resection (fig4).
Fig4
In summary, in our study, we demonstrated how to use the Fluobeam near-infrared real-time imaging system for precise resection of tumors. Moreover, the signal of the fluorescent dye is the strongest at the tumor boundary, and it is also very helpful for the determination of the surgical tumor boundary. Given the excellent performance of the Fluobeam near-infrared real-time imaging system in this study, we believe that near-infrared imaging offers the possibility of real-time guidance for clinical tumor removal surgery.
References: Mieog, JS, et al., Image-guided tumor resection using real-time near-infrared fluorescence in a syngeneic rat model of primary breast cancer. Breast Cancer Res Treat, 2010.